Finding the optimal ventilator settings can be complicated.
What we know:
Although PEEP may improve oxygenation, it can worsen ventilation-perfusion ratios and gas exchange by decreasing cardiac output and tissue oxygen delivery that contribute to impaired arterial oxygenation in patients with increased shunt fractions [7].
Helping clinicians personalize ventilation.
Optimize Ventilator Settings.
Gain bedside insights into the effects of changes in lung health to personalize lung protective strategy
Source: Amboss, 2022
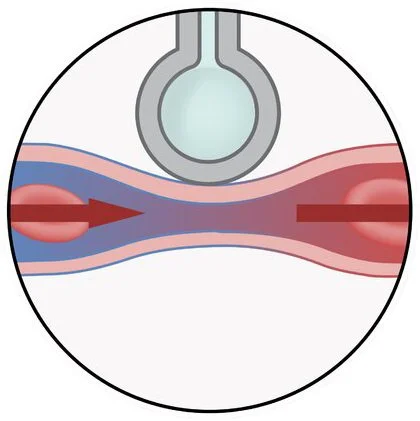
Shunt Perfusion (Low V/Q)
Perfusion of poorly ventilated alveoli or wasted ventilation (e.g. airway obstruction, pneumonia).
Source: Amboss, 2022
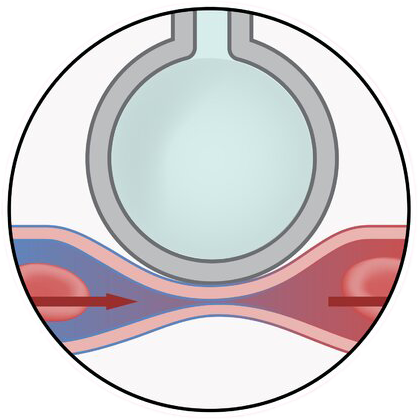
Normal V/Q
The pulmonary circulation of a patient can be regulated to match the ventilation of the alveoli in order to optimize gas exchange.
Dead Space (High V/Q)
Ventilation of poorly perfused alveoli or wasted ventilation (e.g. pulmonary embolism, cardiogenic shock).
Source: Amboss, 2022
ATTENTION: The VQm® is Health Canada approved. The VQm® is not available for sale in any other jurisdiction including the USA and Europe. Any descriptions of functionality are for informational purposes only and reflect only the currently approved product. Product availability remains at Rostrum Medical’s discretion, is subject to change without notice, and is subject to applicable regulatory clearances or approvals.
-
1. Battaglini, D., Sottano, M., Ball, L., Robba, C., Rocco, P., & Pelosi, P. (2021). Ten golden rules for individualized mechanical ventilation in acute respiratory distress syndrome. Journal of Intensive Medicine.
2. Rimeika D, Sanchez-Crespo A, Nyren S, Lindahl SG, Wiklund CU. Iloprost inhalation redistributes pulmonary perfusion and decreases arterial oxygenation in healthy volunteers. Acta Anaesthesiol Scand. 2009 Oct;53(9):1158-66.
3. Sawheny E, Ellis AL, Kinasewitz GT. Iloprost improves gas exchange in patients with pulmonary hypertension and ARDS. Chest. 2013 Jul;144(1):55-62
4. Gattinoni, L., et al., Positive end-expiratory pressure: how to set it at the individual level. Annals of Translational Medicine, 2017. 5(14): p. 288.
5. Diamond M, Peniston Feliciano HL, Sanghavi D, et al. Acute Respiratory Distress Syndrome. [Updated 2021 Jan 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/nooks/NBK436002/
6. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005 Jun;33(6):1266-71.
7. Çoruh, B., & Luks, A. M. (2014). Positive end-expiratory pressure. when more may not be better. Annals of the American Thoracic Society, 11(8), 1327–1331.
8. Denise Battaglini, Marco Sottano, Lorenzo Ball, Chiara Robba, Patricia R.M. Rocco, Paolo Pelosi, Ten golden rules for individualized mechanical ventilation in acute respiratory distress syndrome, Journal of Intensive Medicine, Volume 1, Issue 1, 2021, Pages 42-51, ISSN 2667-100X, https://doi.org/10.1016/j.jointm.2021.01.003.
9. Rudd, K. E., Johnson, S. C., Agesa, K. M., Shackelford, K. A., Tsoi, D., Kievlan, D. R., Colombara, D. V., Ikuta, K. S., Kissoon, N., Finfer, S., Fleischmann-Struzek, C., Machado, F. R., Reinhart, K. K., Rowan, K., Seymour, C. W., Watson, R. S., West, T. E., Marinho, F., Hay, S. I., Lozano, R., … Naghavi, M. (2020). Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet (London, England), 395(10219), 200–211. https://doi.org/10.1016/S0140-6736(19)32989-7